[Event Report] The 112th HGPI Seminar – The Frontlines of Pain Medicine: Necessary Steps for Building a Multidisciplinary System for Treating Pain (February 8, 2023)
date : 5/9/2023
Tags: Chronic Pain, HGPI Seminar, NCDs
![[Event Report] The 112th HGPI Seminar – The Frontlines of Pain Medicine: Necessary Steps for Building a Multidisciplinary System for Treating Pain (February 8, 2023)](https://hgpi.org/en/wp-content/uploads/sites/2/hs112-top_JPNENG-1.jpg)
For the 112th HGPI Seminar, we hosted Mr. Kazuho Wakazono, who is Representative Director of the Goodbye Pain Patient Support Organization for Intractable Neuropathic Pain; and Professor Shoji Yabuki of Fukushima Medical University’s Department of Pain Medicine. They discussed the latest evidence in the treatment of chronic pain, domestic and international efforts to construct multidisciplinary treatment systems, and current issues and other topics related to Japan’s treatment system.
Key points of the lecture
- The 2020 revision of the definition of pain from the International Association for the Study of Pain (IASP) defines pain as something that is impacted by psychosocial factors and that it does not always correspond to tissue damage.
- There are limits to treating pain with the conventional biomedical model. Treating pain requires a multidisciplinary approach based on the biopsychosocial (BPS) model.
- While efforts to establish comprehensive pain centers for providing multidisciplinary treatment for pain are advancing in Japan and overseas, such efforts face challenges in Japan that prevent multidisciplinary treatments from being provided or expanded in a continuous manner. For example, such treatments are not covered in the medical service fee schedule.
- Japan lacks sufficient evidence regarding various treatments for pain, including for multidisciplinary treatments. Research on the effectiveness of those treatments must be advanced.
- Chronic pain is an issue that spans multiple professions, diseases, and fields of medical specialty. It will be necessary to hold discussions with diverse stakeholders and enact a Basic Act on Chronic Pain Measures to provide a strong legal backing for actions that aim to address the complex issue of chronic pain.
The updated definition of pain and global trends in applying the biopsychosocial (BPS) model for the treatment of pain
We usually think of pain as something that accompanies tissue damage to serve as a warning sign to avoid more serious injury. As such, during conventional medical consultations for people with pain, medical staff focused on finding injured tissue and providing treatments for those injuries. However, there are cases in which tissue damage heals but pain remains. This sort of pain is considered to be “chronic pain” and is known as something that is difficult to treat. Chronic pain is related to psychological and social factors (for example, environmental factors in school or the workplace), so treating it requires methods based on the BPS model instead of the conventional biomedical model.
Regarding global developments in this area, the International Association for the Study of Pain (IASP) revised its definition of pain in 2020. In addition to pointing out that pain does not always correspond to tissue damage and that it has an emotional aspect, the updated definition emphasizes that pain can be influenced by various BPS factors and to varying degrees. In response to this progress in pain research, the World Health Organization (WHO) updated its handling of the term “chronic pain” in the International Statistical Classification of Diseases 11th Revision (ICD-11). While pain was previously handled as a symptom, the ICD-11 now classifies chronic pain as an independent disease.
The latest evidence related to chronic pain treatment
Evidence has been presented for various methods of treating chronic pain, from pharmacotherapy to interventional pain management and non-pharmacological therapies. The study group behind the “Research Program for Achieving Equity in Chronic Pain Treatment Systems and Better Healthcare Using a Database of Pain Treatment Centers” compiled guidelines for the treatment of chronic pain in 2021. Those guidelines sort chronic pain treatments into six main categories and offer recommended priority levels for each, which are described below.
- Pharmacotherapy: Recommendation level 2
While Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) are effective for chronic low back pain (CLBP) and osteoarthritis of the knee, their effectiveness is minimal, so they have been assigned recommendation level 2. Long-term use of NSAIDs can also lead to kidney damage or cause other side effects, so they must be used with caution.
- Trigger point injections (TPI): Recommendation level 2
Treatment through trigger point injections (TPIs) is provided by injecting local anesthesia at trigger points, which are tender areas of the body. TPIs have been reported to be effective, so they have been designated recommendation level 2. At the same time, as an invasive procedure, TPIs must not be administered aimlessly.
- Rehabilitation and exercise therapy: Recommendation level 1
The relief of pain through exercise therapy is called “exercise-induced hypoalgesia.” Because exercise-induced hypoalgesia has been reported to relieve pain without side effects, it has been assigned recommendation level 1. Research on the underlying mechanism of this form of pain relief is currently advancing. In one proposed mechanism, exercise increases the production of cannabinoids in the brain to suppress pain. In another, it is suppressed through myokines produced by the muscles. At the same time, improvements in quality of life (QOL) that can be obtained by exercise therapy alone are limited.
- Psychotherapy and Cognitive Behavioral Therapy (CBT): Recommendation level 2
Cognitive Behavioral Therapy (CBT) has been recognized as effective for pain from multiple angles. At the same time, efforts to create a domestic CBT provision system have fallen behind. While there is insufficient evidence for CBT in Japan, an important perspective to foster during treatment is the idea that people can live with pain rather than only pursuing pain relief or the factors causing it. That is to say, people require support to avoid exacerbating pain or developing chronic pain due to negative thinking, which is called “catastrophic thinking.”
- Integrated treatment: Recommendation level 2
Acupuncture has been reported to be effective for treating chronic pain and has been assigned recommendation level 2. When selecting treatment methods, it is desirable that patents’ values are prioritized while taking effectiveness and cost into account.
- Multidisciplinary treatment: Recommendation level 2 (For lower back pain, recommendation level 1)
In this form of treatment, a number of therapies are combined through multidisciplinary intervention. Multidisciplinary treatment has been shown to be effective for intractable pain that has been diagnosed to have no effective methods of treatment. For over two decades, Fukushima Medical University has been using the liaison approach to provide multidisciplinary treatment. In that approach, a number of specialists collaborate on treatment and include clinical psychologists, psychiatrists, pharmacists, nurses, physiotherapists, and social workers. They are visited by patients who have been told that no treatment options are available at other hospitals, and about half of them report improvements to pain and QOL.
Good examples of pain treatment systems overseas
There is broad understanding toward the need for a treatment system that involves multidisciplinary collaboration to provide evidence-based treatments for pain, and efforts to establish pain centers are now advancing in each country. By 2013, many Western countries had already established such multidisciplinary pain centers where multidisciplinary specialists collaborate on treatments. The number of multidisciplinary pain centers continues to increase in many countries. Looking at examples in East Asia, we see that in China, hospitals above a certain size are required to establish departments for pain that provide multidisciplinary treatments for pain from multiple specialists.
One innovative example of unified action for pain among pain centers and employment support services comes from Washington in the U.S. There, people with chronic pain after experiencing workplace injuries are treated at rehabilitation hospitals to help them return to work. Treatment is provided over four weeks of combined exercise and occupational therapy provided by internists, physical therapists, occupational therapists, and clinical psychologists. This program has been extremely effective with 75.8% of people returning to work after one year.
A large-scale massive awareness-building campaign for the concept of pain on the number of injury claims and a case study on how it affected medical costs
There have also been reports of innovative efforts being made overseas to disseminate information to the public. For example, Australia launched a large-scale media campaign aimed at helping more people live without lower back pain. It featured celebrities and experts who provided the latest, evidence-based information in an accessible manner to educate the public on the importance of staying physically active without worrying too much about existing lower back pain. It helped more people with lower back pain pursue more active lifestyles and was reported to result in a decline in the number of claims for CLBP by 15% and to reduce medical costs for CLBP by 20%. As we can see, much attention is being paid to chronic pain in other countries that are providing examples of innovative initiatives to create treatment systems and build awareness among the public.
Helping people avoid becoming “pain refugees” who cannot receive suitable treatment or support in Japan
In one survey, 22.5% of Japanese people reported experiencing chronic pain rated five or higher on a ten-point scale and that lasted three months or more. From this finding, it was estimated that 23 million adults in Japan live with chronic pain, meaning this is an issue that affects an extremely large number of people. Since the enactment of the Cancer Control Act in Japan, recognition has grown toward the importance of helping people with cancer manage pain in addition to treating the cancer itself, and more proactive approaches to treating pain are now being taken. However, there are many cases where adequate treatments are not being provided even for people experiencing severe pain. In particular, many people with long-term pain that has no identifiable cause end up becoming what are known as “pain refugees” because they have nowhere to go to receive appropriate treatments. These include people with fibromyalgia, Complex Regional Pain Syndrome (CRPS), pain after spinal cord injury, and severe non-specific low back pain. Addressing problems facing pain refugees will require an appropriate understanding that chronic pain is holistic and treating it requires collaboration across specialties.
Issues facing the creation of a domestic healthcare provision system that is based on the BPS model
Chronic pain involves various factors and addressing it requires a multidisciplinary approach involving various specialists and physicians. A number of underlying issues have resulted in a lack of a collaborative system for providing multidisciplinary treatment in Japan that include the siloed structure of each medical department, insufficient knowledge regarding chronic pain, and failure to keep pace with the latest knowledge in this area.
Even when treatments have been proven to be effective from multiple perspectives, Japan lacks a system for effectively utilizing them for pain, resulting in poor access. For example, providing psychotherapy or CBT is costly in terms of human capital, which means health institutions are unable to generate sufficient revenue for its costs. Similar issues lie behind the failure for the multidisciplinary collaboration needed to provide multidisciplinary treatments to become widespread.
At multidisciplinary pain centers in Japan, treatment is provided through collaboration that involves various specialists, but reimbursement through the medical service fee schedule is insufficient when multiple professionals are involved in treatment over long periods. This makes it difficult to sustain treatment. While chronic pain treatment guidelines recommend combining multiple therapies including exercise therapy and psychotherapy, there is no evidence for the treatment programs being provided in Japan or their content. To take steps to update the medical service fee schedule so it assigns sufficient points to cover the costs of treatment from multidisciplinary teams, it will be important for us in Japan to publish high-quality papers that demonstrate the effectiveness of multidisciplinary treatments.
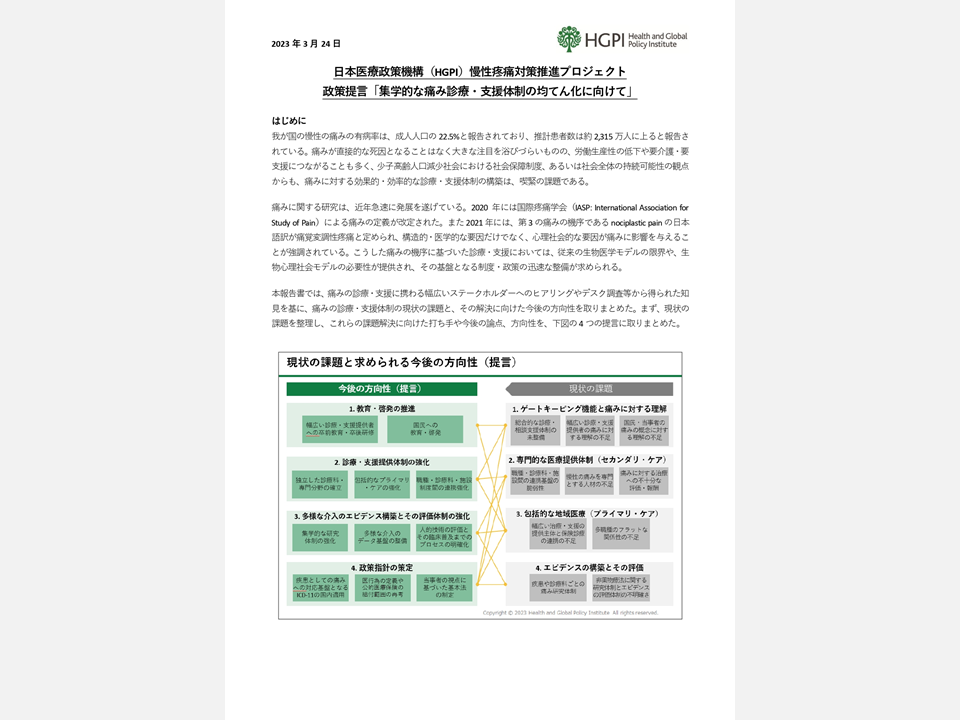
Domestic trends in measures for chronic pain and the need to formulate a Basic Act on Chronic Pain Measures
A number of policies related to chronic pain measures have been advanced in Japan. In 2010, an MHLW study group on chronic pain pointed out addressing chronic pain will require integrated, multidisciplinary treatments that transcend the frameworks of health specialties. That was followed by ongoing research projects, and efforts to establish multidisciplinary pain centers are now advancing under an MHLW research group for the “Research Project on Chronic Pain Policy.” That initiative certifies facilities as “multidisciplinary pain centers” after confirming they have established systems that assess pain, and determine treatments through multidisciplinary conferences and provide multidisciplinary treatments. While there were 23 certified facilities in 2019, that number was increased to 38 facilities as of March 2023.
A number of other efforts have been taken for chronic pain. In addition to the establishment of the Parliamentary Association for Chronic Pain Measures, scientific findings were shared with the legislature to mark a meeting of the International Association for the Study of Pain being held in Japan. Non-partisan Diet Member study groups on chronic pain have also been held. In addition, statements on the promotion of measures for chronic pain were included in the “Plan for Promoting Dynamic Engagement of All Citizens” approved by Cabinet decision in June 2016 as well as in the 2017 and 2018 versions of the Basic Policy on Economic and Fiscal Management.
Recent years have seen remarkable medical and scientific advances for pain. We must further accelerate related political developments to rapidly establish treatment systems that keep pace with scientific progress. Many of the issues related to measures for chronic pain should be broadly disseminated to build understanding among citizens and establish a better chronic pain treatment system that takes into account the unique characteristics of Japan as soon as possible. This will require promotion in legal terms by formulating a Basic Act on Chronic Pain Measures through discussions that have broad participation from related parties.
[Event Overview]
■ Speakers (in Japanese syllabary order):
– Shoji Yabuki (Dean, Department of Physical Therapy, School of Health Sciences, Fukushima Medical University; (Concurrent) Professor, Endowed Chair, Department of Pain Medicine, Fukushima Medical University; (Concurrent) Professor, Department of Orthopaedic Surgery, Fukushima Medical University)
– Kazuho Wakazono (Representative Director, the Goodbye Pain Patient Support Organization for Intractable Neuropathic Pain)
■ Date and time: Wednesday, February 8, 2023; 18:30 – 20:00 JST
■ Format: Online (Zoom webinar)
■ Language: Japanese
■ Participation fee: Free
■ Capacity: 500
■ Profiles:
Shoji Yabuki (Dean, Department of Physical Therapy, School of Health Sciences, Fukushima Medical University; (Concurrent) Professor, Endowed Chair, Department of Pain Medicine, Fukushima Medical University; (Concurrent) Professor, Department of Orthopaedic Surgery, Fukushima Medical University)
After graduating from the School of Medicine at Fukushima Medical University, Professor Shoji Yabuki joined the Department of Orthopaedic Surgery at that same university. He then visited Gothenburg, Sweden, where he studied at Gothenburg University. He was later appointed to various positions including Head of Orthopedic Surgery, Fukushima Prefectural Tsukitakata Hospital; Visiting Professor, University of California, San Diego; Associate Professor, School of Medicine, Fukushima Medical University; and Director, Rehabilitation Center, Fukushima Medical University Hospital (until June 2014). His current roles include Professor of Orthopedics, School of Medicine, Fukushima Medical University (since 2011); Professor, Endowed Chair, Department of Pain Medicine, School of Medicine, Fukushima Medical University (since 2015); and Dean, Department of Physical Therapy, School of Health Sciences, Fukushima Medical University (since 2021).
In 2022, he was appointed head of the research team on the “Study on Improving Healthcare Through Equity in the Chronic Pain Treatment System Centered on Pain Clinics and the Utilization of Medical Databases.”
Professor Yabuki has served as a committee member or board member at a number of academic societies. His current positions include Board Member, the Japanese Association for the Study of Pain; President, the Japanese Association for the Study of Musculoskeletal Pain; and Secretary, Tohoku Region, the Japanese Association for Rehabilitation Medicine.
Kazuho Wakazono (Representative Director, the Goodbye Pain Patient Support Organization for Intractable Neuropathic Pain)
Mr. Kazuho Wakazono began serving as a teacher at a public elementary school in Gifu Prefecture in 1981. In 2011, while still teaching, he founded an organization called the National Association for Patients with Chronic Pain After Spinal Cord Injury, which he serves as Representative. In 2013, he retired from teaching early to focus on his efforts to achieve better healthcare for chronic pain and became Representative Director of the Goodbye Pain Patient Support Organization for Intractable Neuropathic Pain. He also served as Representative of the Japan Hemp Council in the Study Group on Countermeasures Against Marijuana and Other Drugs in 2021, a role in which he continues to work to protect Japan’s hemp culture while preventing drug abuse.
Top Research & Recommendations Posts
- [Policy Recommendations] Reshaping Japan’s Immunization Policy for Life Course Coverage and Vaccine Equity: Challenges and Prospects for an Era of Prevention and Health Promotion (April 25, 2025)
- [Research Report] Perceptions, Knowledge, Actions and Perspectives of Healthcare Organizations in Japan in Relation to Climate Change and Health: A Cross-Sectional Study (November 13, 2025)
- [Research Report] The 2025 Public Opinion Survey on Healthcare in Japan (March 17, 2025)
- [Research Report] The 2026 Public Opinion Survey on Healthcare in Japan (February 13, 2026)
- [Research Report] 2019 Survey on Healthcare in Japan
- [Research Report] Building a Mental Health Program for Children and Measuring its Effectiveness (June 16, 2022)
- [Policy Recommendations] Developing a National Health and Climate Strategy for Japan (June 26, 2024)
- [Research Report] The Public Opinion Survey on Child-Rearing in Modern Japan (Final Report) (March 4, 2022)
- [Research Report] The 2023 Public Opinion Survey on Satisfaction in Healthcare in Japan and Healthcare Applications of Generative AI (January 11, 2024)
- [Policy Recommendations] Mental Health Project: Recommendations on Three Issues in the Area of Mental Health (July 4, 2025)
Featured Posts
-
2026-01-09
[Registration Open] (Hybrid Format) Dementia Project FY2025 Initiative Concluding Symposium “The Future of Dementia Policy Surrounding Families and Others Who Care for People with Dementia” (March 9, 2026)
![[Registration Open] (Hybrid Format) Dementia Project FY2025 Initiative Concluding Symposium “The Future of Dementia Policy Surrounding Families and Others Who Care for People with Dementia” (March 9, 2026)](https://hgpi.org/en/wp-content/uploads/sites/2/dementia-20260309-top.png)
-
2026-02-27
[Registration Open] (Webinar) The 142nd HGPI Seminar “World Kidney Day 2026” Theme in Focus: The Current State of Green Nephrology and Green Dialysis—Balancing Kidney Health and Planetary Health (March 10, 2026)
![[Registration Open] (Webinar) The 142nd HGPI Seminar “World Kidney Day 2026” Theme in Focus: The Current State of Green Nephrology and Green Dialysis—Balancing Kidney Health and Planetary Health (March 10, 2026)](https://hgpi.org/en/wp-content/uploads/sites/2/The142nd_HGPI_Seminar.jpg)
-
2026-03-03
[Registration Open] Online Seminar “Implementing Chronic Kidney Disease (CKD) Measures into Society: Towards a Data-Driven Health System” (April 21, 2026)
![[Registration Open] Online Seminar “Implementing Chronic Kidney Disease (CKD) Measures into Society: Towards a Data-Driven Health System” (April 21, 2026)](https://hgpi.org/en/wp-content/uploads/sites/2/HGPI_20260421_CKDonlineseminar-.png)