[Event Report] 1st Chair’s Dialogue Session “Introduction to Public-Private Partnerships – Global Case Studies in the Healthcare Sector” (May 9, 2025)
date : 7/16/2025
Tags: HGPI Seminar
![[Event Report] 1st Chair’s Dialogue Session “Introduction to Public-Private Partnerships – Global Case Studies in the Healthcare Sector” (May 9, 2025)](https://hgpi.org/en/wp-content/uploads/sites/2/1st-HGPI-Chairs-Dialogue-Session.pptx-1.png)
This seminar series was launched to provide an open forum for discussion and dialogue on key issues in healthcare and health policy in Japan and around the world. Each session features a global leader in the healthcare field either from Japan or abroad who delivers a lecture on a specific theme, followed by a dialogue with the Chair of Health and Global Policy Institute (HGPI).
In the inaugural session, we welcomed Dr. Andy Poh, Senior Fellow at HGPI and Honorary Professor at the University of Birmingham. Dr. Poh delivered a keynote presentation on public-private partnerships (PPPs) in the healthcare sector. Following his lecture, he engaged in a dialogue with Mr. Ryoji Noritake, Chair of HGPI, facilitating a multifaceted exchange of perspectives.
<POINTS>
- In PPPs, it is essential to clearly define crucial parameters such as roles, responsibilities, risk allocation and investment, based on the premise that both sectors benefit in a meaningful collaboration.
- In the healthcare sector, various PPP models exist, including infrastructure-focused, service delivery, and integrated models. When implementing PPPs, it is important to design and apply the most suitable model by taking into consideration each context’s healthcare challenges, institutional frameworks and funding considerations.
- To address the contemporary dynamics and complex challenges faced by healthcare systems, such as technological advancements, widening social disparities and the impact of climate change, PPPs can evolve beyond transactionally-based approaches towards co-creation of new possibilities and systems. There is growing expectation for the promotion of next generation PPPs that prioritize public value, equity, and resilience, by leveraging on the rise of emerging technologies.
■ The video is available (English only)
■ Public-Private Partnerships in the Healthcare Sector
Public-private partnerships (PPPs) generate and result in mutual benefits, such as ameliorating the quality, efficiency and innovation of public services, as well as enhancing their sustainability and resilience.
PPPs refer to long-term contractual relationships in which the public and private sectors work together to develop public infrastructure and provide public services, making use of each other’s strengths. While there is no standard, internationally-accepted definition, the World Bank defines PPPs as typically a long-term contract between a private party and a government agency for providing a public asset or service, in which the private party bears significant risk and management responsibility.
PPPs offer benefits to both the public and private sectors. For the public sector, advantages include improvements in the quality, efficiency and innovation of public services; access to new sources of funding; risk sharing and access to critical skills and expertise. For the private sector, benefits include acquiring new market share, enhancing business sustainability, reducing risks and expanding the scale or scope of operations over the long term. To ensure mutual benefits, it is essential to clearly define roles and responsibilities and to appropriately allocate risks between the two sectors.
The Importance of Implementing Optimal PPP Models that Reflect Local Healthcare Needs and the Strengths of Public and Private Sectors
There are multiple models of PPPs. An objective way of understanding such models can be to consider different factors, including the scale of investment from the private sector and the degree of responsibility it assumes, as illustrated in Figure 1 – a PPP classification model (Source: UNESCAP). In the healthcare sector, PPPs can be categorized into three types: (1) infrastructure-based models, in which the private sector is responsible for facility construction, financing and non-clinical services; (2) clinical service-based models, which involve the provision of clinical services; and (3) hybrid models, which incorporate both infrastructure and clinical service components.
The applicability of PPP models is highly dependent on the social, institutional and funding contexts of the region in which they are introduced. The choice of a specific model can be determined based on the healthcare challenges to be addressed and the expected outcomes of the partnership. For instance, factors such as the need to address shortages in local healthcare service provision, relevance of expertise between the public and private sectors, requirement of respective investment, degree of operational autonomy and risk-sharing mechanism all posit critical determinants in model selection. Designing and implementing the most suitable PPP model requires careful consideration of these contextual factors. The following section presents several successful case examples of PPPs in healthcare that have been designed and implemented in alignment with the local healthcare needs, institutional and financial considerations.
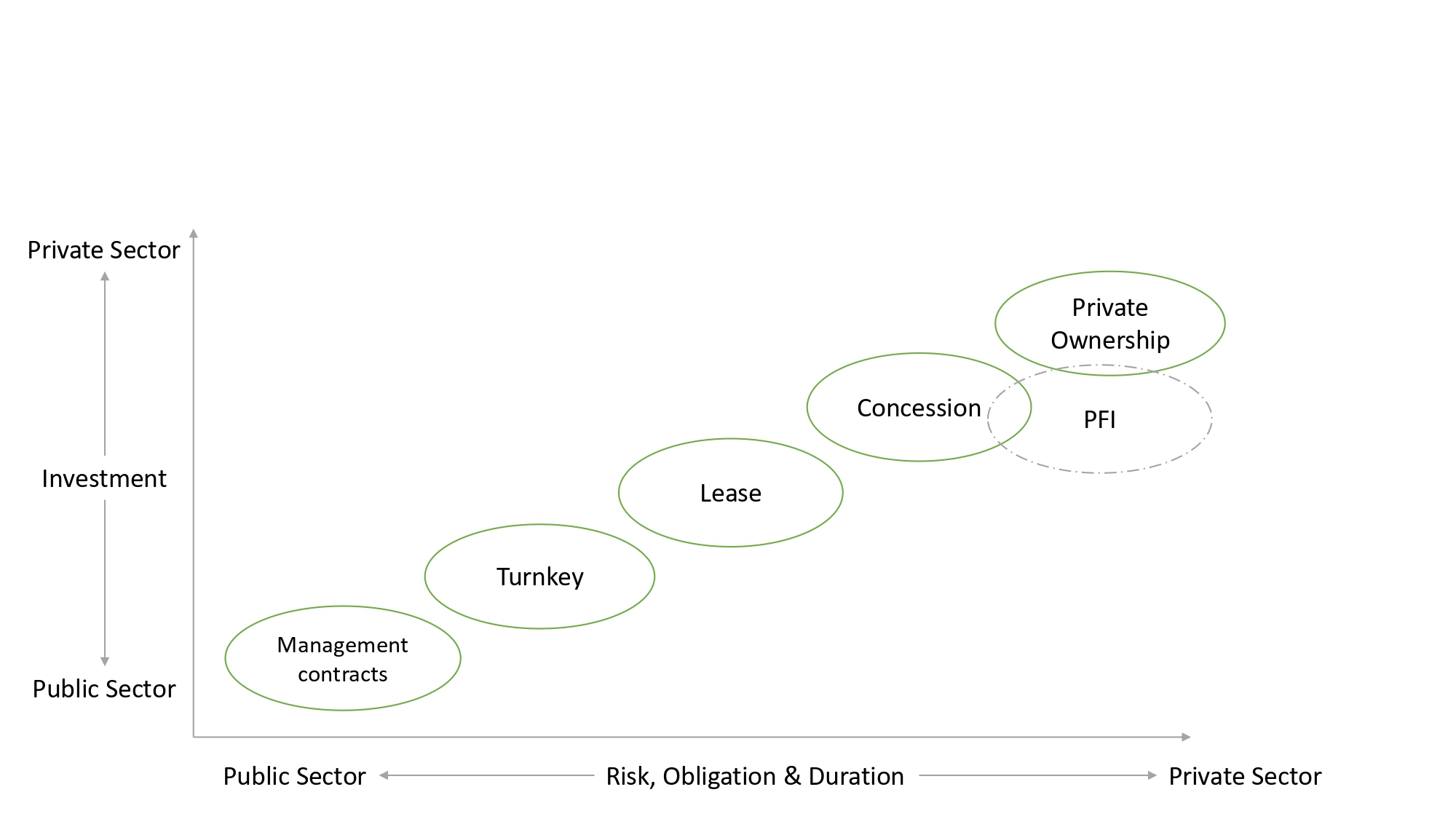
Figure 1. Classification of Public-Private Partnership Models by the United Nations Economic and Social Commission for Asia and the Pacific (UNESCAP) (UNESCAP, 2011)
―Global Case Studies of Public-Private Partnerships in Healthcare―
Rwanda: AI-Driven Digital Health PPP
In Rwanda, a PPP was established between the government and a private technology company to reinforce access to affordable healthcare services through the use of digital technologies. To achieve this, the Rwandan Ministry of Health collaborated with a local subsidiary of a UK-based telemedicine company to roll out a nationwide telehealth service powered by Artificial Intelligence (AI). The initiative has been particularly effective in improving access to healthcare in rural areas, where medical infrastructure is limited. This case is regarded as an international example of AI-powered telehealth PPP. It demonstrates how digital technologies can significantly improve healthcare delivery with impact on a large-scale.
Spain: The Alzira Model (Integrated Care PPP)
Whilst no longer operational, the Alzira Model represented an integrated public-private partnership implemented in Valencia, Spain. Under a long-term concession arrangement, a private consortium was responsible for operating healthcare services, including the hospital and primary care network. The government provided a capitation-based payment to the private operator, ensuring stable revenue while requiring the achievement of outcomes-based performance targets, such as quality and efficiency of care. This model emphasized collaboration among key stakeholders, including the public sector (government) and the private sector (operating consortium). The model highlighted patient-centered care outcomes as a key performance criterion. Although the partnership model has since not been renewed by the government, the Alzira Model is still a notable healthcare PPP example. It offers valuable insights and lessons in building a “win–win” framework for both public and private entities.
■ Discussion with the Chair of HGPI
In the latter half of the session, Mr. Ryoji Noritake, Chair of HGPI, engaged in an invigorating dialogue with Dr. Andy Poh to build on the presentation in the first half. The discussion began by acknowledging that today’s healthcare systems face changing developments and increasingly complex challenges, such as rapid technological advancements, widening social disparities and the growing impact of climate change, which may require new thinking beyond conventional PPPs. Against this backdrop, the two speakers explored the need for next-generation PPPs that place public value, equity and resilience at their core, while actively leveraging on technology and evidence-based data. They emphasized the importance of reimagining PPPs not merely as tools for project implementation, but as catalysts for co-creating public value and advancing systemic reform. The discussion concluded with a forward-looking perspective, by underlining the critical role of cross-border PPPs in preparing for future global health crises and newer models which co-create dynamic, citizen-centered ecosystems with game-changing technologies.
[Event Overview]
- Speaker: Dr. Andy Poh (Senior Fellow, Health and Global Policy Institute)
- Date: Friday, May 9, 2025
- Format: Online
- Language: English
■ Profile
Andy Poh (Senior Fellow, Health and Global Policy Institute)
From Singapore, Professor Andy Poh is a seasoned Healthcare Strategist, Executive, Leadership and Transformation Advisor with an international career of senior-level positions across government and industry. His roles include advising country-level and organizational leadership on strategy, policy, system-level transformation and the future of healthcare systems.
Among his diverse appointments, he is Senior Fellow at the Health and Global Policy Institute, Honorary Professor at the University of Birmingham, Senior Advisor to World Scientific Publishing and Senior Advisor in the Board of Advisors of Health System Intelligence, an international entity which specializes in cutting-edge capabilities of predictive healthcare AI-data analytics. He has been longstanding Advisor in the Prime Minister’s Office of the United Arab Emirates. Earlier, he worked in the Government of Dubai at the Dubai Health Authority with roles of strategic transformation and business innovation. Prior to the UAE, he was based in Singapore and China as Vice President and General Manager of a listed healthcare group, growing its network and leading overseas market expansion via greenfield and brownfield strategies. He first started his career as a doctor practicing medicine in Australia and Singapore. He has attained graduate qualifications in Medicine, Law, Public Administration, Business Administration and Education.
Top Research & Recommendations Posts
- [Policy Recommendations] The Path to a Sustainable Healthcare System: Three Key Objectives for Public Deliberation (January 22, 2026)
- [Research Report] The 2025 Public Opinion Survey on Healthcare in Japan (March 17, 2025)
- [Research Report] Perceptions, Knowledge, Actions and Perspectives of Healthcare Organizations in Japan in Relation to Climate Change and Health: A Cross-Sectional Study (November 13, 2025)
- [Research Report] The 2023 Public Opinion Survey on Satisfaction in Healthcare in Japan and Healthcare Applications of Generative AI (January 11, 2024)
- [Policy Recommendations] Reshaping Japan’s Immunization Policy for Life Course Coverage and Vaccine Equity: Challenges and Prospects for an Era of Prevention and Health Promotion (April 25, 2025)
- [Policy Recommendations] Developing a National Health and Climate Strategy for Japan (June 26, 2024)
- [Policy Recommendations] Achieving Equity in Multidisciplinary Pain Treatment and Support Systems for Pain Management (March 31, 2023)
- [Public Comment Submission] “Assessment Report on Climate Change Impacts in Japan (Draft Overview)” (December 24, 2025)
- [Research Report] The Public Opinion Survey on Child-Rearing in Modern Japan (Final Report) (March 4, 2022)
- [Research Report] Survey of Japanese Physicians Regarding Climate Change and Health (December 3, 2023)
Featured Posts
-
2026-01-09
[Registration Open] (Hybrid Format) Dementia Project FY2025 Initiative Concluding Symposium “The Future of Dementia Policy Surrounding Families and Others Who Care for People with Dementia” (March 9, 2026)
![[Registration Open] (Hybrid Format) Dementia Project FY2025 Initiative Concluding Symposium “The Future of Dementia Policy Surrounding Families and Others Who Care for People with Dementia” (March 9, 2026)](https://hgpi.org/en/wp-content/uploads/sites/2/dementia-20260309-top.png)
-
2026-02-05
[Registration Open] (Webinar) The 141st HGPI Seminar “Current Status and Future Prospects of Korea’s Obesity Policy: Voices of People with Lived Experience in Policy Promotion” (March 3, 2026)
![[Registration Open] (Webinar) The 141st HGPI Seminar “Current Status and Future Prospects of Korea’s Obesity Policy: Voices of People with Lived Experience in Policy Promotion” (March 3, 2026)](https://hgpi.org/en/wp-content/uploads/sites/2/hs141-top-1.png)
-
2026-02-06
[Research Report] AMR Policy Update #5: Cancer Care and AMR (Part 2)
![[Research Report] AMR Policy Update #5: Cancer Care and AMR (Part 2)](https://hgpi.org/en/wp-content/uploads/sites/2/HGPI_20260204_AMR-Policy-Update-5.png)