[HGPI Policy Column] (No.42) — From the Chronic Pain Project “Policies for Chronic Pain by The Scottish Government”
date : 4/26/2024
Tags: Chronic Pain, HGPI Policy Column, NCDs
![[HGPI Policy Column] (No.42) — From the Chronic Pain Project “Policies for Chronic Pain by The Scottish Government”](https://hgpi.org/en/wp-content/uploads/sites/2/column-42-top.png)
<POINTS>
- In Scotland in 2021, the Scottish Government committed to working with local, regional and national stakeholders, including patient groups to develop a national approach to service delivery for chronic pain acknowledging the high prevalence of chronic pain and its impact and the importance of prioritising policy development.
- A large number of people with lived experience participated in Scotland’s National Advisory Committee for Chronic Pain within the government to discuss policies aligned with the needs of people living with pain.
- Surveys, the activities of the third sector, and the active engagement of patients and health care professionals in meetings illuminated the diverse needs of individuals from various backgrounds, integrating them into the policymaking process.
- Policy discussions encompassed a spectrum of pain causes, addressing both complex pain and less complex pain, which often presents alongside one of more other long-term conditions.
Introduction
In recent years, advancements in neuroscience have led to a better understanding of the pain mechanisms and the accumulation of evidence for pain management. On the other hand, it has been a global public health challenge to reflect this new evidence into service delivery. Mainly in developed countries, there is a growing movement to reassess previous pain management services and formulate national strategies pertaining to pain, with the aim of promoting pain treatments tailored to each individual’s condition based on the latest available evidence in pain science.
In Japan, a parliamentary group on chronic pain management was established in 2014, engaging in ongoing discussions with the goal of enacting the Basic Law for Chronic Pain Management. Additionally, starting from the fiscal year 2023, there has been an increase in momentum for establishing national strategies in Japan, chief of which can be seen in the petition aiming at enacting the law. On the other hand, stakeholders related to pain management exhibit a diverse range of interests, making it challenging to reach a consensus. Treatments and care for pain-triggering diseases, diversely ranging from complex pain such as fibromyalgia, to common diseases such as cancer, orthopaedic diseases, neurological diseases and autoimmune diseases, are supplied by various medical departments and health professionals.
How did countries that successfully establish national pain strategies navigate dialogues with stakeholders holding different orientations and formulate policies? This column will introduce the case of Scotland, which in 2022 compiled a national framework entitled “Framework for pain management service delivery”[i] and subsequently an Implementation Plan for the Framework.[ii]
Summary of the Scottish Government’s Framework and Scotland Service Model
Scotland Service Model[iii]
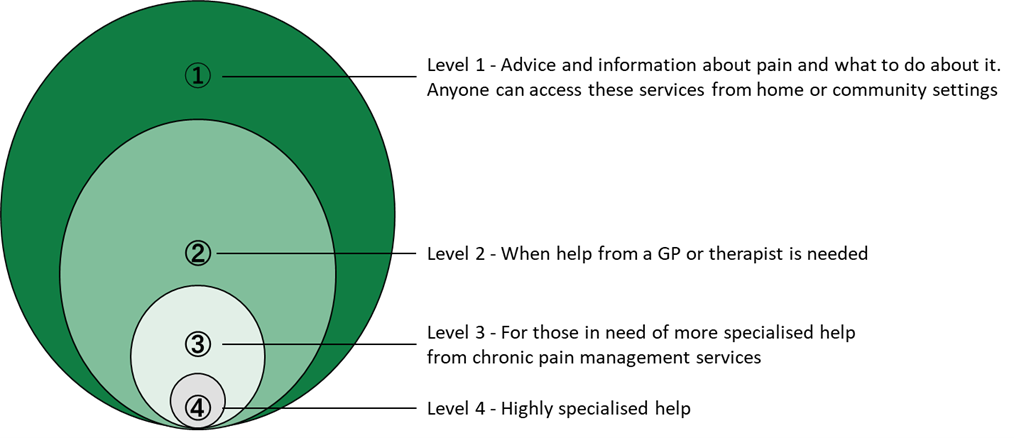
The Scottish Service Model for Chronic Pain, announced in 2014, stratifies pain care at different levels within Scotland, taking into account the complexity of pain and the diverse providers of care. This model has been adopted by the Scottish government, serving as the cornerstone of Scotland’s approach to chronic pain policy.
- Level 1: Care in communities based on the patient’s self-management.
- Level 2: Care provided by local general practitioners (GPs) and therapists for low-complexity pain.
- Level 3: Specialised and interdisciplinary treatment for moderate-complexity pain.
- Level 4: Advanced pain management programmes for high-complexity pain.
Figure 1: Model of care. (Gilbert S, Holdsworth L, Smith B. The Scottish model for chronic pain management services. British Journal of Healthcare Management December 2014;20(12):568-577.)
Scottish Government’s Framework
To strengthen the delivery of care based on the individual’s need, “framework for pain management service delivery – implementation plan” compiled the voices of people with lived experience into the four actions needed:
A: Patient-cantered care
B: Access to care
C: Safe and effective support
D: Improvement of the quality of services and care
Enablers of the National Framework Development
- Establishment of a platform for multi-stakeholder discussions
Platform for discussions at the Cross-party Group (CPG) on Chronic Pain
The Cross-party Group (CPG) on Chronic Pain in Scotland was founded in 2001. It is dedicated to actively promoting awareness of the ongoing challenges confronted by individuals experiencing chronic pain. Its primary objective is to enhance the provision of speedy and appropriate treatment and care. Under the leadership of parliamentarians, over 200 individuals and organisations, including a broad range of patients and citizen groups, healthcare providers, academia, and industry stakeholders, have been involved, paving the way for diverse stakeholders to engage in discussions. Even after the Scottish Government responses to chronic pain initiated the CPG remains a vital forum for discussions. This ensures the voices of the diverse stakeholders of chronic pain are heard.
Platform for discussion in the Scottish Government
Following debates within the parliamentary group, in 2014, the Minister of Public Health founded the National Chronic Pain Improvement Group. Subsequently, in 2017, a committee within the Scottish Health Department, known as the National Advisory Committee for Chronic Pain (NACCP), was established. These committees comprise individuals dedicated to the governance of public institutions and healthcare establishments, including academic professionals. Furthermore, members encompass healthcare providers of diverse specialisations and disciplines, alongside representatives of a broad spectrum of health conditions. Collectively, they have engaged in thoughtful deliberations, discussing pain treatment approaches with the aim of reaching a consensus.
Such a collaborative structure has been put into practice during the implementation stage following the 2022 framework formulation. The Pain Management Task Force, which directly provides information to the relevant ministers, involves a diverse range of stakeholders related to healthcare and welfare, including individuals directly affected by pain. In addition, measures have been instituted to ensure the inclusion of diverse stakeholder perspectives. These include the establishment of a Lived Experience Panel[iv], comprising individuals with first-hand experience in pain management, and the implementation of a reporting system through Health Improvement Scotland to articulate the voices of individuals.
Figure 2: Governance arrangements for implementation of the Framework. (Scottish Government, 2022. Framework for pain management service delivery – implementation plan.)
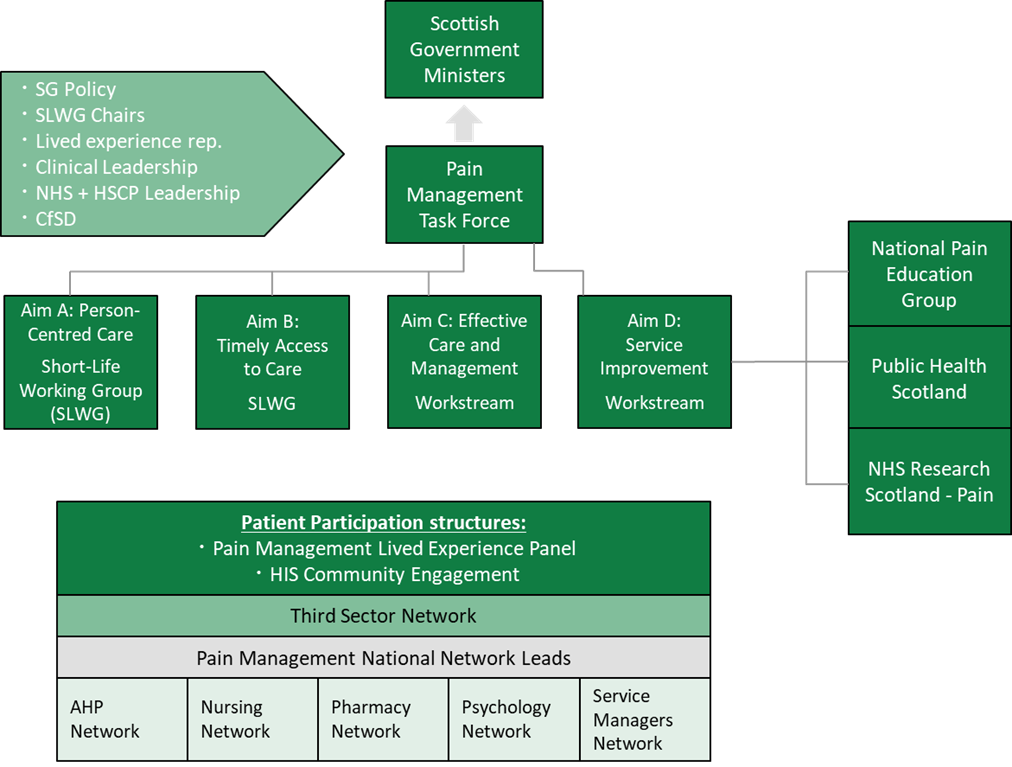
*SG: Scottish Government, NHS: National Health Service, HSCP: Health and Social Care Partnership, CfSD: the national Centre for Sustainable Delivery, HIS: Health Improvement Scotland, AHP: Allied Health Professional
- Contributors to delivering voices of patients with different diseases to policies
Collecting diverse voices through civic organisations
In the United Kingdom, charitable activities led by civic organisations, “the Third Sector”, are actively taking place. For example, Pain Concern, which held a commissioner role at NACCP, disseminates information about pain in an understandable format for patients and citizens, and also provides consultation support for those experiencing pain. The Third Sector plays an important role in channelling the collective voices of people with lived experience through consultation support services, thereby influencing policies. Simultaneously, it makes individual contributions to each person living in pain. Such initiatives by the third sector, including those by Chronic Pain Australia in Australia and counterparts in other countries, contribute to advancing policies from the perspective of the third sector that works closely to those directly affected.
Epidemiological Surveys on Chronic Pain
Throughout these processes, a diverse array of stakeholder voices has shaped policy influence. However, there is a growing awareness that the voices heard in these processes only reveal a small part of the whole picture, underscoring the need to understand the existing circumstances of a broader range of patients. To reinforce that, epidemiological research has contributed to understanding epidemiology and associated factors of chronic pain. As an example, a review on chronic pain epidemiology in population-based studies were published in 2019[v]. It reported the high prevalence and incidence of chronic pain as well as summarised various factors of chronic pain which include demographic, lifestyle and behaviour, clinical and other factors. Understanding the diverse factors of chronic pain calls for the comprehensive management of its causes and effects, which can be other health conditions including mental health and other multi-morbidities, at both individual and population levels.
Implications for Japan
In Japan, similar initiatives have taken place to get across the collective perspectives of patients with various diseases through the involvement of patient organisations. This includes active participation in parliamentary groups and petition campaigns, supported by multiple patient organisations. To make further policy advancements in the inclusion of patients and citizens, Japan is expected to institute a specialised consultation support system dedicated to pain management, amplify individual voices and visualise the needs of those navigating pain by drawing inspiration from existing initiatives.
[i] Scottish Government. Chronic pain service delivery – draft framework: consultation. 2022. Available from: https://www.gov.scot/publications/draft-framework-chronic-pain-service-delivery/pages/1/ (Viewed on February 24, 2024)
[ii] Scottish Government. Framework for pain management service delivery implementation plan. 2022. Available from: https://www.gov.scot/binaries/content/documents/govscot/publications/strategy-plan/2022/07/framework-pain-management-service-delivery-implementation-plan/documents/framework-pain-management-service-delivery-implementation-plan/framework-pain-management-service-delivery-implementation-plan/govscot%3Adocument/framework-pain-management-service-delivery-implementation-plan.pdf (Viewed on February 24, 2024)
[iii] Gilbert S, Holdsworth L, Smith B. The Scottish model for chronic pain management services. British Journal of Healthcare Management December 2014;20(12):568-577. Available from: https://doi.org/10.12968/bjhc.2014.20.12.568 (Viewed on February 24, 2024)
[iv] Scottish Government, 2022. Scottish Government Pain Management Panel. Available from: https://www.gov.scot/binaries/content/documents/govscot/publications/independent-report/2022/11/scottish-government-pain-management-panel/documents/scottish-government-pain-management-panel/scottish-government-pain-management-panel/govscot%3Adocument/scottish-government-pain-management-panel.pdf (Viewed on February 24, 2024)
[v] Mills SEE, Nicolson KP, Smith BH. Chronic pain: a review of its epidemiology and associated factors in population-based studies. Br J Anaesth. 2019 Aug;123(2):e273-e283. Available from: http://doi.org/10.1016/j.bja.2019.03.023 (Viewed on April 1, 2024)
Acknowledgement
We sincerely appreciate Dr Blair H. Smith, Professor at University of Dundee; the former National Lead Clinician for Chronic Pain, Ms Nicola Rhind, Clinical Specialist Physiotherapist, Grampian Pain Management Service; the National Lead Clinician for Chronic Pain, and the Scottish Government Chronic Pain Policy Team for their kind supports when compiling this column.
Authors
Takahiro Sakauchi (Manager, HGPI)
Yuri Isoda (Intern, HGPI)
Top Research & Recommendations Posts
- [Policy Recommendations] Achieving a Sustainable Society of Health and Longevity Through the Integration of Environment and Healthcare-Incorporating a Planetary Health Perspective into the 3rd Phase of The Healthcare Policy-(December 20, 2024)
- [Research Report] Building a Mental Health Program for Children and Measuring its Effectiveness (June 16, 2022)
- [Policy Recommendations] Integrating Climate and Health for a Sustainable Society: Incorporating a Planetary Health Perspective into Nationally Determined Contributions (NDCs)(December 9, 2024)
- [Policy Recommendations] Developing a National Health and Climate Strategy for Japan (June 26, 2024)
- [Policy Recommendations] Policy Recommendations on Strengthening CKD Strategies for Workers: The Importance of Providing Early Detection, Intervention, and Support Through Screenings and Medical Visits (October 28, 2024)
- [Research Report] The 2023 Public Opinion Survey on Satisfaction in Healthcare in Japan and Healthcare Applications of Generative AI (January 11, 2024)
- [Event Report] Planetary Health Expert Meeting Aiming for Sustainable Healthcare: Learning from the Impact of Environmental Pollution and Medical Waste During the Pandemic (February 16, 2024)
- [Policy Recommendations] Obesity Control Promotion Project 2023 “The Next Steps for Engaging and Cooperating with Patients, Citizens, and Communities for Implements of Obesity Control Measurements” (April 8, 2024)
- [Announcement] A Turning Point Towards Building Green Healthcare Systems (June 5, 2024)
- [Research Report] Survey of Japanese Physicians Regarding Climate Change and Health (December 3, 2023)
Featured Posts
-
2024-11-25
[Registration Open] (Webinar) The 130th HGPI Seminar “Marking a Decade of the Act on Medical Care for Patients With Intractable Diseases: Connecting Intractable Diseases and Society From the Perspective of a Media Professional and Family Member” (January 28, 2025)
![[Registration Open] (Webinar) The 130th HGPI Seminar “Marking a Decade of the Act on Medical Care for Patients With Intractable Diseases: Connecting Intractable Diseases and Society From the Perspective of a Media Professional and Family Member” (January 28, 2025)](https://hgpi.org/en/wp-content/uploads/sites/2/hs130-top_JPNENG-1.png)
-
2024-12-18
[Policy Recommendations] Policy Recommendations on Strengthening CKD Strategies for Workers: The Importance of Providing Early Detection, Intervention, and Support Through Screenings and Medical Visits (October 28, 2024)
![[Policy Recommendations] Policy Recommendations on Strengthening CKD Strategies for Workers: The Importance of Providing Early Detection, Intervention, and Support Through Screenings and Medical Visits (October 28, 2024)](https://hgpi.org/en/wp-content/uploads/sites/2/HGPI_20241023_FY2024CKD_eyecatch.jpg)
-
2024-12-20
[Policy Recommendations] Achieving a Sustainable Society of Health and Longevity Through the Integration of Environment and Healthcare-Incorporating a Planetary Health Perspective into the 3rd Phase of The Healthcare Policy-(December 20, 2024)
![[Policy Recommendations] Achieving a Sustainable Society of Health and Longevity Through the Integration of Environment and Healthcare-Incorporating a Planetary Health Perspective into the 3rd Phase of The Healthcare Policy-(December 20, 2024)](https://hgpi.org/en/wp-content/uploads/sites/2/e8a714648913193b03d5b6ede38c161e.png)
-
2024-12-25
[Registration Open] (Hybrid Format) Expert Meeting “Innovations Required to Achieve Precision Psychiatry” (January 22, 2025)
![[Registration Open] (Hybrid Format) Expert Meeting “Innovations Required to Achieve Precision Psychiatry” (January 22, 2025)](https://hgpi.org/en/wp-content/uploads/sites/2/mh-20250122-topr-1.png)
-
2024-12-27
[Activity Report] Second UN General Assembly High-Level Meeting on AMR (September 26, 2024)
![[Activity Report] Second UN General Assembly High-Level Meeting on AMR (September 26, 2024)](https://hgpi.org/en/wp-content/uploads/sites/2/4ED86AF7-49DE-465D-B59D-843B4F3C6102_1_201_a-scaled-1.jpeg)