[Event Report] The 96th HGPI Seminar – The Current Situation for Cognitive Behavioral Therapy (CBT) and Future Prospects for the Dissemination of CBT (July 1, 2021)
date : 8/12/2021
Tags: HGPI Seminar, Mental Health
![[Event Report] The 96th HGPI Seminar – The Current Situation for Cognitive Behavioral Therapy (CBT) and Future Prospects for the Dissemination of CBT (July 1, 2021)](https://hgpi.org/en/wp-content/uploads/sites/2/hs96-top_ENG.jpg)
For the 96th HGPI Seminar, we hosted Dr. Hironori Kuga, Director of the National Center for Cognitive Behavior Therapy and Research at the National Center of Neurology and Psychiatry (NCNP). Dr. Kuga provided an overview on CBT, trends in related domestic policies, and activities, and future prospects for the spread of CBT.
<Key points of the lecture>
- Cognitive Behavior Therapy (CBT) is a form of psychotherapy that promotes more realistic and balanced thinking as well as positive emotions and behavior by altering cognition (the way people think about and perceive things).
- Many people are experiencing stress due to the Coronavirus Disease 2019 (COVID-19) pandemic. Providing support through services that utilize digital technologies and support in communities or workplaces will be important to ensure mental health treatments reach people during the pandemic. Expectations are high for the use of the cognitive-behavioral approach when providing that support.
- Evidence for CBT has also been established in Japan. Starting in FY2010, CBT became eligible for reimbursement in the medical service fee schedule. That schedule currently covers the use of CBT for six targeted diseases.
- The National Center for Cognitive Behavior Therapy and Research at the NCNP is Japan’s first training and research center specializing in CBT. Aiming to improve the quality of psychiatric care techniques used in Japan to achieve a society that provides better psychiatric care services to more people, its activities are centered on three pillars: research, training, and clinical activity support.
■ Trends in policies related to CBT
Coverage for CBT in the medical service fee schedule
Cognitive Behavior Therapy (CBT) is a form of psychotherapy developed by American psychiatrist Professor Aaron Beck in the 1960s that aims to promote more realistic and balanced thinking as well as positive emotions and behavior by altering cognition (the way people perceive and think about things). In recent years, interest in CBT has also grown in Japan, where it is being used in various fields like education, industry, law, and community mental health in addition to the field of healthcare.
In Japan, the Ministry of Health, Labor and Welfare (MHLW) conducted a study to demonstrate the safety and effectiveness of CBT called “Research on Psychotherapy Methods and Their Effectiveness” as part of the Research Project on Psychiatric and Neurological Diseases and Mental Health from 2007 to 2009. It then created the “Cognitive Therapy and Cognitive-Behavioral Therapy for Depression Treatment Manual.” Based on evidence generated through these initiatives, CBT was made eligible for reimbursement in the FY2010 revision of the medical service fee schedule when provided to people other than those receiving inpatient treatment for depression and other mood disorders.
Since then, evidence for the use of CBT in treating other diseases has also been established. In addition to depression and other mood disorders, the medical service fee schedule currently covers the use of CBT for a total of six diseases: obsessive-compulsive disorder, social anxiety disorder, panic disorder, post-traumatic stress disorder, and bulimia nervosa. As for practitioners, only physicians were eligible for reimbursement until the FY2016 revision of the medical service fee schedule. After that revision, reimbursement for CBT became possible when treatment is provided by nurses with a certain level of knowledge and experience under the direction of and in collaboration with physicians. Certain facility requirements for nurses to provide CBT were relaxed in the FY2018 revision.
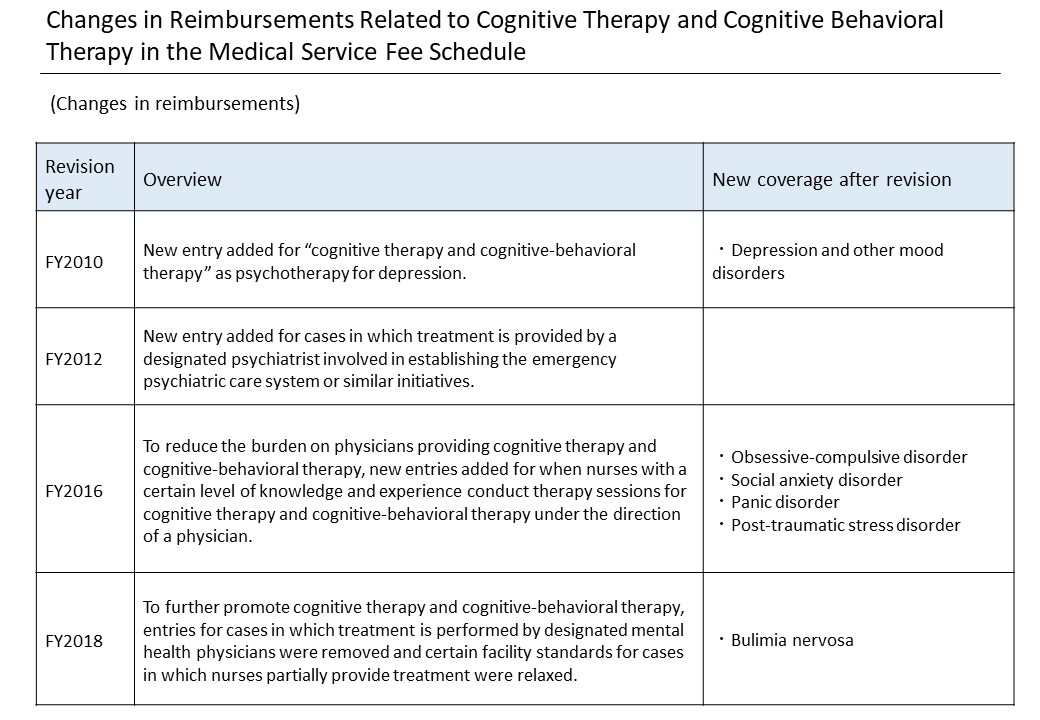
Figure 1. (From lecture materials)
The positioning of CBT in the Medical Care Plan System
The implementation status of CBT has also been included as a key indicator in the seventh revision of the Medical Care Plan System, which is currently in effect. The positioning of mental health care in the Medical Care Plan was also changed. Mental disorders were included among targeted illnesses in 2011, bringing their total up to five (cancer, stroke, acute myocardial infarction, diabetes, and mental disorders). Since the sixth revision of the Medical Care Plan System came into effect in 2013, each municipality has been advancing efforts to identify which healthcare services they require to meet local demand for mental disorder treatment and to create plans to promote the division of roles and collaboration among healthcare institutions.
There are two important pillars in the healthcare system for mental disorders: establishing an integrated community care system that can also respond to mental disorders and establishing a healthcare coordination system that can respond to mental disorders. The construction of “an integrated community care system that can also respond to mental disorders” is currently being promoted so each person can live true to themselves with peace of mind, whether they are affected by a mental disorder or not. Mental disorders encompass a wide variety of illnesses. In addition to mood disorders such as depression, they also include schizophrenia, dementia, and addiction. To respond to the diverse needs of people affected by these disorders, roles must be divided within healthcare provision services for each mental disorder and providers must cooperate with each other.
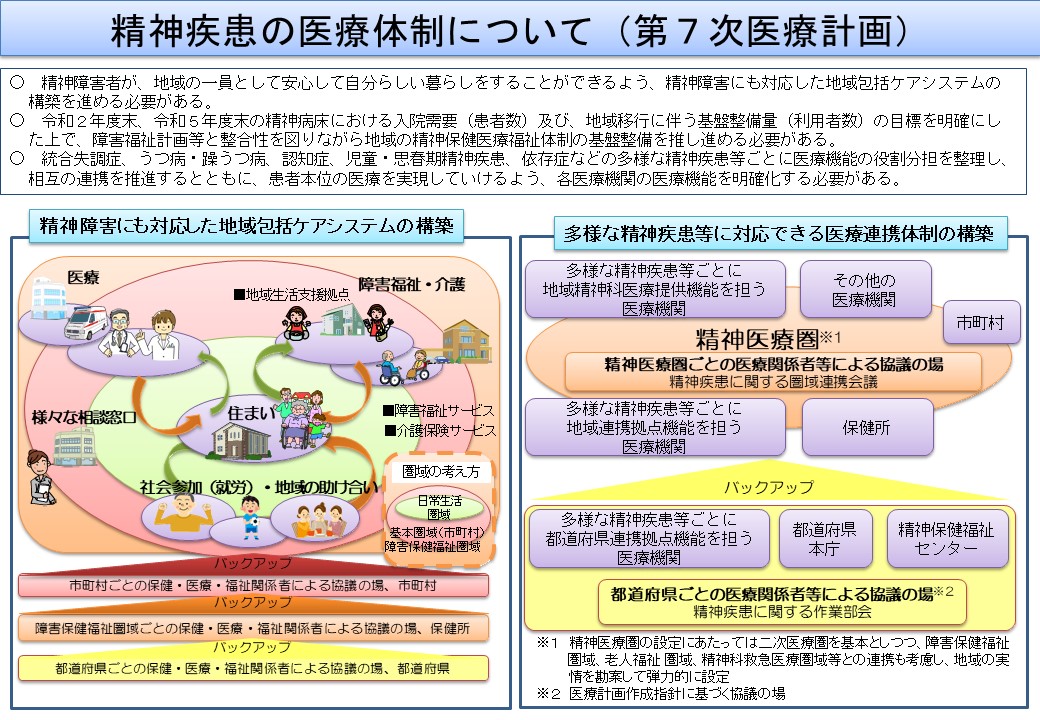
Figure 2. (From lecture materials, Japanese only)
For prefectures to grasp current conditions within their healthcare provision systems and set targets, evaluation indicators will be necessary. The MHLW has provided example indicators from three perspectives: structure, process, and outcomes. Each indicator type is described below.
- Structure indicators measure material resources, human resources, and organizational systems for providing medical services (for example, the number of healthcare institutions providing outpatient schizophrenia treatment).
- Process indicators measure the activities of entities providing services and the systems for cooperating with other organizations (for example, the number of people receiving outpatient schizophrenia treatment).
- Outcome indicators measure the effects of healthcare services on the health in the community (for example, psychiatric care bed discharge rates three, six, and twelve months after hospitalization).
The MHLW’s example indicators included “number of healthcare institutions providing outpatient CBT” and “number of people receiving outpatient CBT” that they encouraged prefectural governments to adopt to grasp and assess the state of systems for providing CBT in their region. However, only seven or eight prefectures have actually adopted these two indicators, so they were made priority indicators during the interim review of the seventh revision of the Medical Care Plan System in 2020.
Current information on progress on these indicators and the state of social resources (healthcare institutions, disability welfare service centers, home nursing care, etc.) in each region can be viewed in the Regional Mental Health Resources Analyzing Database (ReMHRAD), so interested parties are encouraged to access it.
■ The past activities of the National Center for Cognitive Behavior Therapy and Research
Research activities
The NCNP National Center for Cognitive Behavior Therapy and Research is Japan’s first training and research center specializing in CBT. Its operations are centered on the three pillars of research, training, and clinical activity support with the goal of improving the quality of psychotherapy techniques used in Japan to create a society in which more people can access better psychiatric care services. This fiscal year, the Center plans to expand its focus to include medical education by providing collaborative courses with graduate schools in Japan.
Research at the Center emphasizes fields in which further progress is desirable and includes the development of treatments for highly prevalent, intractable, and rare diseases as well as efforts to verify the effectiveness of those treatments. Its researchers are also working to identify psychotherapy’s mechanism of action using magnetic resonance imaging (MRI) and other tools as well as to develop and provide CBT using information and communication technology (ICT) in collaboration with research institutions in Japan and abroad.
The Center is also engaged in clinical activities. Working together with the NCNP National Center Hospital, we provide outpatient CBT to meet the needs of each patient. Through those activities, we have also conducted research to demonstrate the effectiveness of CBT for reducing medication use or for treating a variety of disorders. In a study on people with depression and anxiety disorders, we were able to demonstrate the effectiveness of CBT in reducing amounts of anxiolytic medications compared to initial diagnoses. We also demonstrated CBT’s effectiveness for various disorders including anxiety disorder, obsessive-compulsive disorder, and developmental disorders.
Training and clinical activity support
The National Center for Cognitive Behavior Therapy and Research has provided several training programs since around ten years ago. We also serve as the secretariat of the MHLW’s CBT training project. Our broad range of training programs span beginner to advanced courses and include focused courses for specific disorders or areas of application.
The MHLW CBT training project initially focused on depression but was expanded as more disorders were granted coverage in the medical service fee schedule. It now offers programs for many other disorders. Training starts with a two-day workshop. After that, trainees must complete sixteen sessions with a supervisor 1 and attend a brush-up workshop. As of FY2020, the two-day workshops have been attended by about 6,300 people. Among them, about 440 people have completed supervised sessions. About half of trainees are physicians, but there are also many clinical psychiatric technicians and nurses. Despite these efforts, there are still shortages of CBT specialists in various fields. To meet society’s needs, further efforts to develop human resources are necessary.
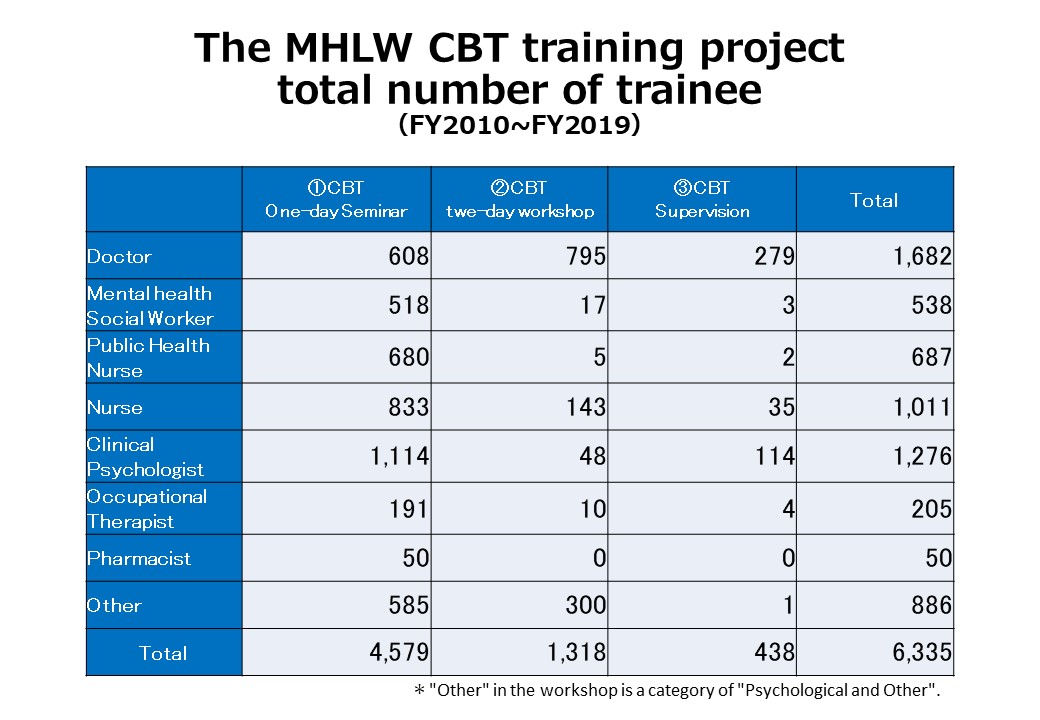
Figure 3. (From lecture materials)
Although the training project has been running for about ten years, its effectiveness has not yet been verified. To verify it, Health and Global Policy Institute (HGPI) conducted a project entitled “Assessing the State of Cognitive Behavior Therapy (CBT) Use in Japan and Examine Systems for Contributing to the Future Dissemination of CBT and CBT-based Practices” as part of the FY2020 MHLW Project for the Promotion of Comprehensive Welfare for Persons with Disabilities (Third Stage) in 2020. Following that research, HGPI created a project report and issued policy recommendations. Using concepts from dissemination and implementation science, those recommendations arranged topics for the future dissemination of CBT into six categories: (1) evidence; (2) policy guidelines; (3) human resources development; (4) provision systems; (5) perspectives of patients and other affected parties; and (6) evaluation and monitoring. They also advocate for the need to consider measures based on these perspectives.
(Please see here for details: [Activity Report] Project Report – HGPI Mental Health Policy Project to Assess State of Cognitive Behavior Therapy (CBT) Use in Japan and Examine Systems for Contributing to the Future Dissemination of CBT and CBT-based Practices as Part of Ministry of Health, Labour and Welfare Project (April 14, 2021))
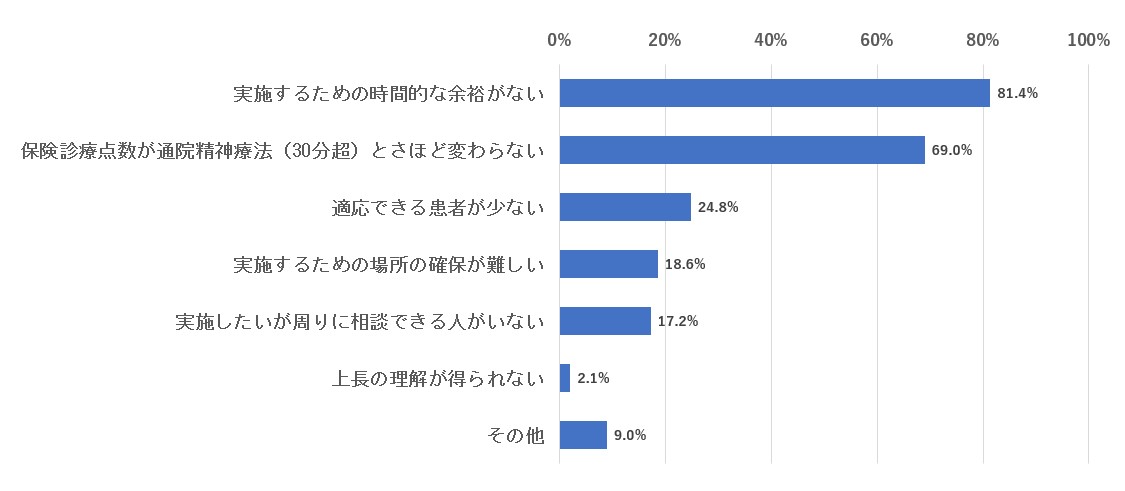
HGPI’s report also mentions time constraints faced by physicians as a factor limiting the dissemination of CBT. When the project’s questionnaire survey asked physicians why they were unable to provide CBT in clinical settings, over 80% of all respondents said they “do not have enough time.”
Difficulties faced by physicians when providing CBT in clinical settings (n=145)
Figure 4. FY2020 MHLW Project for the Promotion of Comprehensive Welfare for Persons with Disabilities (Third Stage) “Assessing the State of Cognitive Behavior Therapy (CBT) Use in Japan and Examine Systems for Contributing to the Future Dissemination of CBT and CBT-based Practices” project report, pp. 48. (Japanese Only)
Treatment with CBT usually consists of ten to twenty face-to-face sessions that last 40 to 50 minutes each. However, according to a 2016 MHLW survey, the average time spent per patient when providing outpatient psychiatric care is less than ten minutes. This shows that even if there is sufficient recognition toward the need for CBT among physicians, the rising number of people receiving outpatient treatment means they cannot secure enough time for each patient. In other words, the current treatment system makes it difficult for physicians to provide adequate CBT.
Treatments using the cognitive-behavioral approach that can be implemented by physicians in other fields or in a multidisciplinary manner
From the perspective of human resource development, it is also important to disseminate methods based on the cognitive-behavioral approach among physicians in other fields. Our survey found there is an increasing number of people asking primary care physicians in internal medicine and other fields about psychiatric symptoms they are experiencing due to the COVID-19 pandemic, like anxiety and depression. In many of those cases, people with mild psychiatric symptoms or physical comorbidities are seen by internists or other physicians instead of specialists. For cases involving mild symptoms, it may be more effective for those physicians to collaborate with specialists and provide treatments that use the cognitive-behavioral approach and can be provided over short periods. Guidelines in the U.K. even name CBT as the first choice for treating mild psychiatric symptoms. In addition to treating psychiatric symptoms, the cognitive-behavioral approach is also effective for improving medication adherence among people with diabetes and hypertension. This has also led to increased interest in CBT is growing among many professions including physicians from other fields, and they are expressing greater need to learn techniques that are based on CBT. To help address that need, the FY2021 MHLW Sciences Research Project, “Research on Implementing, Disseminating, and Establishing a System for Effective Psychotherapy Using CBT Methodology” is currently underway. Through studies and efforts like that one, we want to continue supporting clinical activities by developing appropriate interventions tailored to patients’ symptoms and conditions and by developing high-quality human resources.
■ Future Prospects
Obtaining a Scientific Understanding of the Underlying Mechanism in the Brain
Further disseminating and advancing CBT will require that we understand the underlying brain mechanism behind it. The effects of CBT vary among practitioners and people who receive it, so identifying the mechanisms of CBT in brain science will be important to standardize quality. Expectations are also high for various applications of CBT, such as for the treatment of physical diseases like chronic pain and irritable bowel syndrome, or in rehabilitation, so it will be necessary to establish more evidence.
Utilizing the cognitive-behavioral approach in mental health treatment
Expectations are also high for the further utilization of methods rooted in the cognitive-behavioral approach. The COVID-19 pandemic has resulted in many changes to our environment, personal relationships, and daily habits, and many people are ill at ease. In a survey conducted by the MHLW, over half of approximately 11,000 respondents reported feelings of anxiety. It is urgent that steps are taken to address mental health issues caused by the COVID-19 pandemic.
The dissemination of digital technologies that utilize the cognitive-behavioral approach
A contact-free consultation system that utilizes digital technology will be important for implementing mental health measures during the COVID-19 pandemic. We are currently conducting a study called “Building a Basic Infrastructure for Emergency Remote Mental Healthcare to Meet Changes in Society Due to COVID-19, etc., and Verifying Its Effectiveness to Promote Practical Application” as part of AMED’s FY2020 Comprehensive Research Project for Policy for Persons with Disabilities. Its goal is the construction of a mental healthcare system that combines AI-based tools and online consultation from counselors. In this program, people seeking treatment first enter their symptoms and other information into an AI chatbot called the “Kokoro Conditioner.” Triage is then conducted based on the results. For people with mild symptoms, psychiatric interventions using the cognitive-behavioral approach are provided by Kokoro Conditioner. People with moderate to severe symptoms are provided Psychological First Aid (PFA) through online consultations with counselors.
Efforts for preventive mental healthcare and health promotion in communities, workplaces, and schools
In addition to the field of healthcare, efforts for mental health in terms of first response, preventive care, and health promotion are also important in settings like communities and workplaces.
To improve mental health in communities, the MHLW launched the Mental Health Supporter Training Project this fiscal year. It aims to provide many people with accurate knowledge about mental health to create communities and workplaces where people with mental health problems are supported. The mental health supporter training process teaches how to support people with mental health problems using the cognitive-behavioral approach. That knowledge will also help people take appropriate measures when they experience mental health problems themselves.
The Ministry of Economy, Trade and Industry (METI) and other ministries are also considering initiatives for improving mental health and wellbeing in workplaces. Occupational injury claims related to mental health have been increasing in recent years and there is a great deal of interest toward how companies are responding to the mental health needs of their employees. Mental health problems experienced by employees are often rooted in communication with superiors, so teaching people communication skills and how to cope with stress using the cognitive-behavioral approach has the potential to relieve symptoms and improve those situations. Furthermore, mental health is closely related to sleep, exercise, diet, and other lifestyle habits, and expectations are high for the use of the cognitive-behavioral approach to help improve those habits.
In countries like the U.K. and New Zealand, platforms are being established to promote mental health measures in companies. It is desirable that a platform that can serve as a guideline for mental health management at companies is established in Japan to help maintain and improve public mental health. The National Center for Cognitive Behavioral Therapy and Research wants to collaborate with stakeholders in industry, Government, and academia and contribute to building that platform.
There is also a growing need to utilize digital technology. We plan to strengthen cooperation with IT venture companies and similar organizations to promote the implementation of tailored, appropriate treatments that use the cognitive-behavioral approach throughout society and to standardize treatment quality. Through these efforts, we hope to help improve the symptoms of people with mental health problems and contribute to better mental health and wellbeing for all.
1 Supervisors provide training and guidance on CBT to people undergoing training.
■ Profile
Dr. Hironori Kuga(Director, National Center for Cognitive Behavior Therapy and Research, National Center of Neurology and Psychiatry)
Dr. Hironori Kuga is a psychiatrist. He holds a Ph.D. in Medicine from the Kyushu University Graduate School of Medicine and a Master of Public Health degree from Johns Hopkins University Bloomberg School of Public Health. After graduating from the Oita University Faculty of Medicine in 2006, he underwent postgraduate clinical training at Aso Iizuka Hospital. There, he earned his certification as a Doctor of Internal Medicine at the hospital’s Department of General Medicine. He has served at the National Hospital Organization Hizen Psychiatric Center’s Department of Psychiatry, as Visiting Clinical Fellow to the U.S. Department of Veterans Affairs West Los Angeles Medical Center, and, starting in 2013, as Director of the National Hospital Organization Hizen Psychiatric Center Day Care Center. During that time, he was dispatched to the U.K. for training as part of the Ministry of Health, Labour and Welfare (MHLW) Acute Psychiatric Care Specialist Training Program. In 2016, he went to the U.S. as a Rotary Foundation International Scholar. While working as a postdoctoral researcher at the Department of Psychiatry and Behavioral Sciences at Johns Hopkins University in the U.S., he earned a Master of Public Health degree from the Johns Hopkins Bloomberg School of Public Health in 2018. After serving as an Academic Researcher at the Johns Hopkins Bloomberg School of Public Health, Dr. Kuga returned to Japan and served as a lecturer at Kyushu University Hospital and in the MHLW’s Social Welfare and War Victims’ Relief Bureau as Associate Director of the Department of Health and Welfare for Persons with Disabilities Mental Health and Disability Health Division. He then assumed his current position. He also serves as Core Supervisor of the MHLW Cognitive Behavioral Therapy Training Program and is scheduled to chair the 22nd Annual Convention of the Japanese Association for Cognitive Therapy in 2022.
Top Research & Recommendations Posts
- [Policy Recommendations] The Path to a Sustainable Healthcare System: Three Key Objectives for Public Deliberation (January 22, 2026)
- [Research Report] The 2025 Public Opinion Survey on Healthcare in Japan (March 17, 2025)
- [Research Report] Perceptions, Knowledge, Actions and Perspectives of Healthcare Organizations in Japan in Relation to Climate Change and Health: A Cross-Sectional Study (November 13, 2025)
- [Policy Recommendations] Reshaping Japan’s Immunization Policy for Life Course Coverage and Vaccine Equity: Challenges and Prospects for an Era of Prevention and Health Promotion (April 25, 2025)
- [Research Report] The 2023 Public Opinion Survey on Satisfaction in Healthcare in Japan and Healthcare Applications of Generative AI (January 11, 2024)
- [Research Report] AMR Policy Update #4: Cancer Care and AMR (Part 1)
- [Public Comment Submission] “Assessment Report on Climate Change Impacts in Japan (Draft Overview)” (December 24, 2025)
- [Policy Recommendations] Developing a National Health and Climate Strategy for Japan (June 26, 2024)
- [Research Report] The Public Opinion Survey on Child-Rearing in Modern Japan (Final Report) (March 4, 2022)
- [Research Report] Survey of Japanese Physicians Regarding Climate Change and Health (December 3, 2023)
Featured Posts
-
2026-01-09
[Registration Open] (Hybrid Format) Dementia Project FY2025 Initiative Concluding Symposium “The Future of Dementia Policy Surrounding Families and Others Who Care for People with Dementia” (March 9, 2026)
![[Registration Open] (Hybrid Format) Dementia Project FY2025 Initiative Concluding Symposium “The Future of Dementia Policy Surrounding Families and Others Who Care for People with Dementia” (March 9, 2026)](https://hgpi.org/en/wp-content/uploads/sites/2/dementia-20260309-top.png)
-
2026-02-05
[Registration Open] (Webinar) The 141st HGPI Seminar “Current Status and Future Prospects of Korea’s Obesity Policy: Voices of People with Lived Experience in Policy Promotion” (March 3, 2026)
![[Registration Open] (Webinar) The 141st HGPI Seminar “Current Status and Future Prospects of Korea’s Obesity Policy: Voices of People with Lived Experience in Policy Promotion” (March 3, 2026)](https://hgpi.org/en/wp-content/uploads/sites/2/hs141-top-1.png)
-
2026-02-06
[Research Report] AMR Policy Update #5: Cancer Care and AMR (Part 2)
![[Research Report] AMR Policy Update #5: Cancer Care and AMR (Part 2)](https://hgpi.org/en/wp-content/uploads/sites/2/HGPI_20260204_AMR-Policy-Update-5.png)